-
Who should keep an eye on drug seizure accounts?
Lots of forfeiture money goes to association outside of public purview; giving checks directly to kids This article is from Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join their free mailing list, as this helps provide more public service reporting. By Bonnie Jean Feldkamp When the Vinton County Fair was canceled…
-
Ohio Department of Job and Family Services tries to bolster its own workforce by posting jobs with no medical benefits in pandemic
This article is from Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join their free mailing list, as this helps provide more public service reporting. By Boniface Womber and Bonnie Jean Feldkamp Amid a raging pandemic, Ohio’s agency responsible for looking out for workers’ welfare has started posting full-time temporary jobs with…
-
The Family Court Judge Who Threatened a Mother With Contempt of Court for Getting Her Child a COVID-19 Test
Ohio juvenile court Judge Timothy Grendell thought coronavirus precautions were overblown, and made sure people knew it. In one case he forbade a mother from getting her children tested for COVID-19. Then, one of them had to go to the emergency room. ProPublica is a nonprofit newsroom that investigates abuses of power. Sign up to…
-
Ohio restaurateurs hope winter and COVID won’t kill them off
This article is from Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join their free mailing list, as this helps provide more public service reporting. By Grant Segall At the Academy Tavern in Cleveland last week, Missy and Wilson Heller shared a table but not a comfort level. “I’m freaked out,” Missy…
-
Capacity inches downward as first Ohioans get COVID vaccine
The Ohio Department of Health released more hospital capacity and equipment numbers yesterday, as the first Ohioans received their first vaccine doses and the U.S. death toll exceeded 300,000.
-
Court hands journalists big Freedom of Information Act win, gun data access
5 media outlets, Harvard Law’s Cyberlaw Clinic, and 16 data journalists, including Eye on Ohio join effort to gain access to federal database records This article is from Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join their free mailing list, as this helps provide more public service reporting. On Thursday, the…
-
Top regulator’s exit raises questions about utility and fossil fuel influence
Critics question whether the former Ohio utility commission chair should have recused himself more often to avoid any appearance of bias. This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism in partnership with the nonprofit Energy News Network. Please join our free mailing list or the mailing list for the…
-
A Cold Covid Christmas in Cleveland
As moratoriums end Dec. 1, need grows for utility assistance; Guide to avoiding shutoffs This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join our free mailing list as this helps us provide more public service reporting. By Rachel Dissell and Conor Morris CLEVELAND, Ohio – The needs of…
-
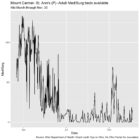
Ohio’s Hospital Capacity Data in Ten Charts
Interactive: Explore Newly Released Hospital Data This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join our free mailing list as this helps us provide more public service reporting. Updated: Additional data from Nov. 21-24 released on Nov. 27. By Lucia Walinchus and Boniface Womber Ohio’s COVID-19 cases are…
-
Ohio Department of Health delays full records release despite court order
33 hospitals report they have no critical care bed and/or medical/surgery bed for adult patients on October 30 This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join our free mailing list as this helps us provide more public service reporting. By Boniface Womber, Bonnie Jean Feldkamp and Kathiann…