-
Breathing easier in Cleveland: How Tighter Standards Could Change the City’s Air Quality Issues
This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join Eye on Ohio’s free mailing list as this helps provide more public service reporting to the community. By Christopher Johnston While running for Cleveland City Council Ward 3 seat last year, Ayat Amin spent a lot of time canvassing…
-
Mental health worker shortage grows in Ohio
This story provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism together with the Cleveland Observer. Please join Eye on Ohio’s free mailing list as this helps provide more public service reporting to the community. Unprecedented demand and a sparse employee pipeline are adding stress to Ohio’s already strained behavioral health system.…
-
Who torched the Hamilton home?
The couple who put their blood, sweat, and tears into building a home to care for their elderly parents and others. The millionaires next door who made it clear they were not welcome. And the dream that mysteriously went up in smoke. This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for…
-
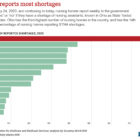
How Ohio became the No. 1 state for nursing home assistant shortages
This story is from the Investigative Reporting Workshop in collaboration with Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join Eye on Ohio’s free mailing list or follow IRW on Facebook as this helps us provide more public service reporting. By Savanna Strott Ohio nursing homes reported more shortages of nursing…
-
Fighting to open closed doors: how advocates stepped up efforts to help sex trafficking survivors in a world where hiding victims is easier than ever
This article is from Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join their free mailing list, as this helps provide more public service reporting. By Christopher Johnston For women survivors of sex trafficking struggling to make ends meet, the COVID-19 pandemic has exacerbated an already desperate situation. Funding programs to support…
-
This Speech Clinic (Literally) Helps Trans People Find Their Voice
This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism in partnership with the Buckeye Flame. Please join our free mailing list or the mailing list for the Flame as this helps us provide more public service reporting. By Caitlin Fisher After beginning with some vocal stretches to warm up her…
-
Dodging disconnection
More help is on the way, but will it be enough? This article is from Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join theirfree mailing list, as this helps provide more public service reporting. By Dan Polletta Janet Cook’s utility bills are stacking up and she doesn’t have enough money to…
-
Ohio Department of Job and Family Services tries to bolster its own workforce by posting jobs with no medical benefits in pandemic
This article is from Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join their free mailing list, as this helps provide more public service reporting. By Boniface Womber and Bonnie Jean Feldkamp Amid a raging pandemic, Ohio’s agency responsible for looking out for workers’ welfare has started posting full-time temporary jobs with…
-
Ohio Department of Health delays full records release despite court order
33 hospitals report they have no critical care bed and/or medical/surgery bed for adult patients on October 30 This article provided by Eye on Ohio, the nonprofit, nonpartisan Ohio Center for Journalism. Please join our free mailing list as this helps us provide more public service reporting. By Boniface Womber, Bonnie Jean Feldkamp and Kathiann…